Written by: Chris Klem, MS (he/him)

As we age, our chances of experiencing some form of trauma increase. By the time we reach retirement, we may have lived for six to nine decades, leaving ample opportunity for hardship and trauma. Given this reality, one might expect that professionals who work with older adults are well-trained in Trauma-Informed Care. However, this assumption is often not true. When we examine programs specifically designed for older adults who are experiencing harm, Trauma-Informed Care is seldom addressed or taught to staff in the aging field. In fact, the term “trauma” is rarely mentioned.
Why is Trauma-Informed Care Lacking in this Field?
Many would agree that abuse and neglect of older adults can lead to significant trauma. Unfortunately, professionals who are responsible for supporting older adult victims often lack training in Trauma-Informed Care. Here are three ideas that illustrate why these concepts may be absent in the aging field:

1. Trauma is frequently associated with experiences from earlier in life, such as childhood trauma, bullying, sexual assault, and domestic violence. There is a common misconception that once individuals reach their sixties or seventies, childhood trauma is in the rear-view mirror, out of sight, out of mind.
2. Another damaging belief is that older adults do not experience trauma from events like domestic violence or sexual assault. In reality, older adults, particularly those with mental health issues or cognitive decline, are at a significantly higher risk of harm. According to the National Council on Aging, one in ten older adults report experiencing abuse, neglect, or exploitation, but only one in twenty-four cases are reported. Furthermore, older adults are rarely referred for therapy, and emotional support is often not prioritized in their care planning.
3. Many professionals working in this field are over-worked and experience daily vicarious trauma or intense feelings of burnout. The combination of these two things can decrease one’s capacity to empathize as a form of self-preservation. Often these programs are stretched thin, and training concepts like “Trauma-Informed Care” are labeled as non-essential and too time-consuming for the front-line staff.
Why Childhood Trauma Matters for Older Adults
The ACE Study (Adverse Childhood Experiences) was a large-scale research project that investigated the effects of childhood abuse, neglect, and other adverse experiences on individuals in adulthood. This study is well-known among professionals in the mental health field who work with both children and adults; however, it often does not reach those who work with older adults. It is important for professionals engaging with older adults to understand post-traumatic stress disorder (PTSD) and complex PTSD (CPTSD), as these conditions can significantly impact an older adult’s life. Additionally, the ACE Study highlighted significant correlations between childhood trauma and physical health issues later in life.

Working with clients who have multiple health conditions, low socioeconomic status, limited education, or unmanaged mental health symptoms requires a deep understanding of how their challenges may be rooted in childhood trauma or complex trauma. Recognizing the impact of ACE scores, Complex PTSD, and an individual’s history of adversity is essential for building strong relationships with our clients. Additionally, the six principles of Trauma-Informed Care offer a framework for professionals to provide high-quality, person-centered care, ultimately leading to improved outcomes for the organization.
Vicarious Trauma and Burnout
When professionals work with victims of abuse and neglect, whether they are children, adults, or older adults, they often experience a high rate of vicarious trauma. This trauma arises from indirect exposure to the victims’ firsthand narratives. These professionals frequently encounter poor living conditions and visible signs of abuse and neglect, and they may even face threats of physical violence themselves.
Working in underfunded programs can also lead workers to develop survival instincts, which can diminish a person’s capacity to hold space for empathy. This unrecognized, and often unsupported form of trauma, can have significant consequences that negatively impact not only the clients, but also the workers and the organizations they are part of. Ongoing, unsupported vicarious trauma can lead to harmful practices, liabilities, and staff turnover.
Why Should Trauma-Informed Care be taught to those working with older adults:

Many professionals in this field are motivated by a genuine desire to help others, often inspired by personal experiences of caring for family members. While their intentions are typically well-meaning, these efforts may not always yield positive outcomes for the clients. Actions perceived as beneficial might not align with what is truly in the client’s best interest and could even lead to significant emotional harm.
Professionals require accessible tools to guide their decision-making, assess risks, and foster supportive environments that prioritize both physical safety and emotional well-being. It is also essential to provide ongoing support to address issues such as vicarious trauma, burnout, and compassion fatigue. Adopting Trauma-Informed Care principles and practices can address these needs, especially when these principles are integrated throughout all levels of an organization and included in annual continuing education.
How do we begin to integrate Trauma-Informed Care?
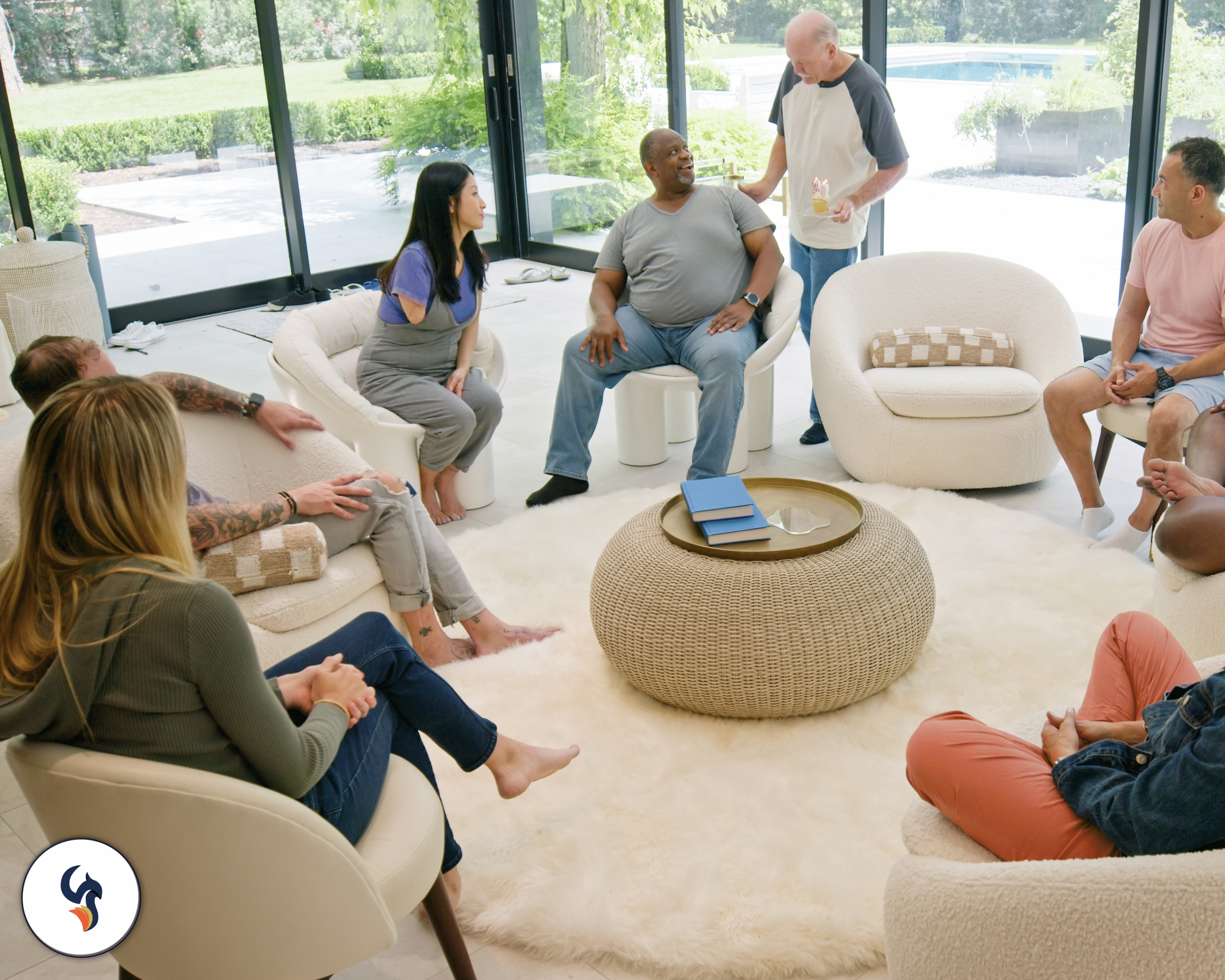
While we may not be able to resolve issues related to funding and caseload sizes, many organizations can improve the training, education, and support they provide to their staff. The six principles of Trauma-Informed Care should be integrated into the onboarding and training of all staff who work with trauma survivors, regardless of their clients’ ages. There have been programs that have made progress over the years and have started incorporating Trauma-Informed Care into their practices, however, these training practices should be the standard across all organizations.
The Phoenix Center offers tailored Trauma-Informed Care training specifically designed to meet the needs of organizations serving older adults. We have trained numerous trauma-focused organizations in the Philadelphia area, including Women Organized Against Rape, the Delaware Coalition Against Domestic Violence, and the Chester County Department of Human Services, among others.
In addition to Trauma-Informed Care training, we also collaborate with teams to develop trauma-informed leadership, foster group cohesion, and enhance workplace wellness. We can assist organizations in recognizing signs of burnout and promoting healthy relationships between leadership and frontline staff. Contact us today to learn more about our workshops and training opportunities.

Written by: Chris Klem, MS (he/him)
Contact: chris@phoenixtraumacenter.com