By: Meryl Lammers, LSW, MT-BC
Is it perimenopause or trauma? Mood swings. Body changes. Brain Fog. Anxiety. Sleeplessness. Why don’t I feel like myself? I don’t recognize my own body. Why does it feel like I’m going through puberty all over again? Why do my joints hurt all the time? Where did my patience go?
If you are in your late 30’s-early 50s and you are a woman or person who menstruates, you may be experiencing perimenopause.
What is Perimenopause?
Perimenopause is the transitional period before menopause. This is a time when bodies of people who menstruate begin to change and prepare for the cessation of menstruation. This phase, which can last for 3-14 years, is characterized by hormonal fluctuations, particularly in estrogen and progesterone levels, leading to various physical and emotional symptoms. These symptoms may include:
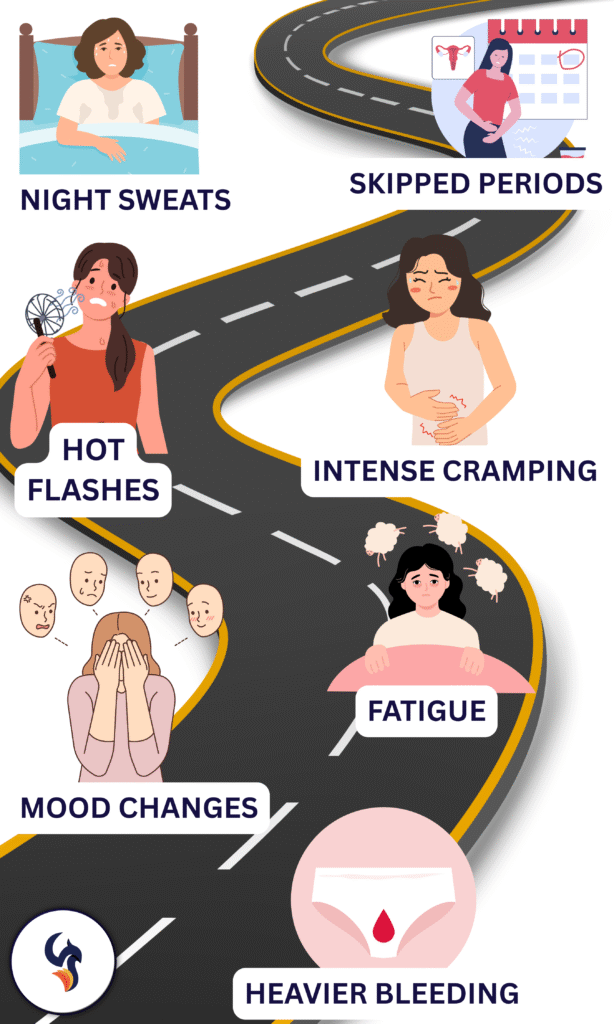
- challenging emotional changes
- sleeping disturbances
- decreased sex drive
- fatigue
- weight gain
- cognitive change
- dry skin
- joint pain
- muscle aches
- headache
- heart palpitations
- changes in taste
- digestive problems
People who have a trauma history may experience more severe perimenopausal symptoms, including hot flashes, sleep disturbances leading to fatigue, difficulty managing emotions, and heightened anxiety and depression.
Perimenopause and Trauma
Studies indicate that people with a history of trauma, particularly during childhood or adolescence, may experience a higher risk of depression and PTSD symptoms during perimenopause. Some red flags to look out for include:
- Increased feelings of depression/loneliness/isolation/anxiety
- Flashbacks of traumatic memories
- Inability to regulate emotions
- Increased suicidal ideation
- Feelings of hopelessness
Perimenopause and Neurodivergence
Is it ADHD or perimenopause? The rising diagnosis rates of neurodivergent conditions, like ADHD and autism, in people undergoing perimenopause is a phenomenon linked to hormonal changes and the impact of masking strategies. The decline of estrogen during perimenopause can worsen symptoms associated with neurodivergence, making previously masked traits more apparent and leading women to seek diagnoses.
Hormonal Changes and Neurodivergence
The hormonal fluctuations during perimenopause can directly impact dopamine regulation, a neurotransmitter crucial for focus and executive function. This can lead to an increase in symptoms like brain fog, forgetfulness, and difficulty concentrating, which are often associated with ADHD. Similarly, for autistic women, hormonal changes can exacerbate sensory sensitivities, social anxiety, and challenges with executive function.
Masking and the “Tipping Point”
Many neurodivergent women may successfully mask or hide their traits for years, particularly in childhood and adolescence. However, the physical and emotional changes of perimenopause, combined with life transitions, can overwhelm existing coping mechanisms. This can lead to a “tipping point” where previously hidden traits become more noticeable, prompting a diagnosis.
Increased Awareness and Intersectional Considerations
Increased awareness about neurodivergence and a shift towards more intersectional diagnoses are also contributing to the rise in late-life diagnoses. Additionally, the physical and emotional symptoms of perimenopause, coupled with the psychological impact of a late diagnosis and potential trauma history can make this transition particularly challenging for neurodivergent people who menstruate.
Where Can I Get Help?
If you…
- believe you are experiencing perimenopausal symptoms, first and foremost contact your medical doctor/gynecologist.
- you are in perimenopause and now curious if you are neurodivergent, please speak to a doctor, psychologist, or psychiatrist who can direct you to health care professionals that conduct neuropsychological examinations for neurodivergence.
- you’re having thoughts of harming yourself or others, please call 988 or 911, or go to your local emergency room.
- you are experiencing an increase in PTSD symptoms or difficulties managing your emotions, experiential trauma therapists are trained to help you through this challenging life transition.
The Phoenix Center
Experiential Trauma Therapy uses evidenced base techniques that can be beneficial for people in perimenopause of all neurotypes who are experiencing these symptoms. Research suggests that somatic or body-based therapies are effective in helping people in menopause cope with trauma. At the Phoenix Center, we specialize in providing EMDR, IFS, Psychodrama, Somatic work, and Creative Expressive Arts, such as music and art therapies, which all have a somatic component. We are here to support you through all life phases!
If you’re ready to get support during this significant life change, contact The Phoenix Center today to schedule with one of our experiential trauma therapists.